Archive
The Birth Control Blues: How The Pill Shapes Your Emotions
Written by Anna Charitonos, May 2025|

Can birth control influence how we feel, think, and make decisions? A recent study out of Utrecht University’s Department of Experimental Psychology suggests it might. Published in late 2024, this study found that hormonal contraceptives – especially the pill – may alter emotional processing, leading to a more ‘flattened’ response to emotions. These findings highlight an important but often overlooked connection between reproductive hormones and mental health. I interviewed Dr. Lotte Gerritsen – a co-author of this paper and researcher at Utrecht University – to get some more insights on what this means for women’s mental health, considering the widespread use of hormonal birth control.
What Inspired This Research?
Previous studies linked the pill to a higher risk of depression, especially in younger users. “This raised so many questions. We really wanted to examine who is vulnerable and when,” Dr. Gerritsen explained. It was unclear whether the negative mood stemmed from young age, an initial mood dip that might resolve with time, or whether those who struggled simply stopped using the pill early on.
How the Pill Affects Emotions
Dr. Gerritsen’s research team looked at electrical activity in the brain and found that women on the pill have a ‘flattened’ emotional response. Imagine emotional variability like a rollercoaster—naturally cycling women experience the highs and lows of a ride, with moments of exhilaration and dips of sadness. In contrast, women on the pill experience emotions more like a train on steady tracks—moving forward but without the same dramatic rises and falls. “Blunting of emotional responses is something many women on hormonal contraceptives recognise,” shared Dr. Gerritsen. However, this isn’t always a bad thing, as Dr. Gerritsen clarified, “some women will fare well on less emotional variability, whereas others actually need the peaks to compensate for their lower than average positive affect.”
The Brain and Hormone Levels: Why Does This Happen?
Estrogen and progesterone are classed as gonadal steroids, but they are not just “sex hormones”. The brain is full of receptors for these chemicals, particularly in areas that play a role in emotion regulation. Although Dr. Gerritsen stated that scientists still do not know why this link between sex hormones and mood exists, studies on how women react and regulate their emotions at different phases of their menstrual cycle have helped us understand how our mood changes as estrogen and progesterone fluctuate.
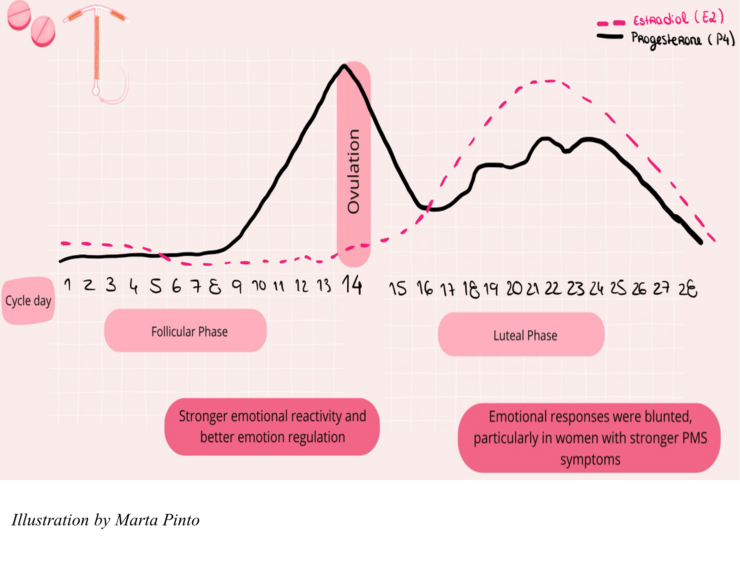
Here you can get a rough idea of how hormones change throughout the average menstrual cycle. The start of a period bleed marks day 1.
Dr Gerritsen’s team also looked into this to compare naturally cycling women to those taking hormonal birth control. In the mid-follicular phase – usually the week just after your period- participants showed stronger emotional reactivity and better emotion regulation. This is the result of estrogen levels rising. In the mid-luteal phase – usually the week just before your period arrives – emotional responses were blunted, particularly in women with stronger PMS symptoms. This is when progesterone dominates.
Why Some Women Feel Fine While Others Struggle
While some women feel moodier or more anxious on birth control, others report greater emotional stability. These differences highlight the flaws in a “one-size-fits-all” approach to prescribing the pill. “It should be more personalized,” Dr. Gerritsen emphasized. She explained that individuals vary in how their bodies regulate natural hormones and metabolize medications, which can influence their response to hormonal contraceptives.
IUD vs. the Pill: Are Some Forms of Birth Control Less Likely to Affect Mood?
While women on the pill exhibited a “blunted” emotional response, those using hormonal IUDs showed emotional patterns more similar to naturally cycling women. Many assume this difference is because the pill affects the whole body, whereas the IUD only releases hormones locally in the uterus. However, this is a misconception. “IUDs also have a systemic effect,” explained Dr. Gerritsen. “Some GPs still ‘sell’ the IUD as a device that only has localized hormonal effects, but that is untrue. The reason we find differences between the IUD and the pill is that IUDs contain only progestin and no synthetic estrogen.”
What This Means for Women’s Health
So, what does this mean for women’s health? How can someone choose the best method to prevent an unwanted pregnancy while also protecting their mental well-being? Awareness of these emotional effects is the first step, but finding the right contraceptive often involves trial and error. Doctors should inform patients about the potential emotional effects of birth control, but self-advocacy is also key. Tracking mood changes when starting hormonal contraception can be helpful, and Dr. Gerritsen advises: “If you experienced depression or anxiety before, please come back to your doctor after three months and do a check-in on how you are feeling.”
Dr. Gerritsen and her research team are contributing to a larger conversation about the stigma surrounding menstruation and the longstanding gaps in women’s health research. To further this point, we can turn to the delayed recognition of PMDD (premenstrual dysphoric disorder) as a clinical mental health condition, reflecting how menstrual-related issues have historically been overlooked. “I think all women should get to know their bodies better. There is still too much shame and shyness when talking about menstruation,” Dr. Gerritsen emphasized. This stigma may have slowed scientific advancements, yet new discoveries—such as the presence of stem cells in menstrual blood—challenge outdated perceptions and highlight the need for more research on the menstrual cycle’s impact on health.
A Hard Pill To Swallow: The Persistent Burden On Women
As research reveals the complex effects of hormonal birth control on the brain, one thing is clear: the burden of contraception, and its potential health trade-offs, falls largely on women. Many are prescribed hormonal methods without full awareness of their emotional impact, highlighting a broader gap in reproductive healthcare. Breaking the stigma around menstruation and contraceptives, while advocating for better education, personalized care, and continued research, is essential. Contraception should not come at the cost of mental well-being—it’s time for a more informed and equitable approach.
Disclaimer
For the sake of simplicity, this article uses woman-specific language. However, the author is aware and acknowledges that not all those who have a menstrual cycle or use hormonal contraceptives identify as women.
Sources
Doornweerd, A. M., Baas, J. M. P., Montoya, E. R., Van De Vijver, I., & Gerritsen, L. (2024). Emotion and birth control: Emotion regulation ERPs differ based on menstrual cycle phase and hormonal contraceptive use. Psychoneuroendocrinology, 170, 107174. https://doi.org/10.1016/j.psyneuen.2024.107174
Petersen, N., London, E.D., Liang, L. et al. Emotion regulation in women with premenstrual dysphoric disorder. Arch Womens Ment Health 19, 891–898 (2016). https://doi.org/10.1007/s00737-016-0634-4
Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø. Association of Hormonal Contraception With Depression. JAMA Psychiatry. 2016;73(11):1154–1162. doi:10.1001/jamapsychiatry.2016.2387
Ulrich, D., Muralitharan, R., & Gargett, C. E. (2013). Toward the use of endometrial and menstrual blood mesenchymal stem cells for cell-based therapies. Expert Opinion on Biological Therapy, 13(10), 1387–1400. https://doi.org/10.1517/14712598.2013.826187
Endometrail stem cells: https://www.the-scientist.com/an-endometrial-stem-cell-pioneer-72146
You must be logged in to post a comment.