The development of artificial organs
How mini-lungs can help us to do research on the coronavirus
Written by Mirte Linthorst
Since the beginning of 2020, the coronavirus has gripped the world. Everyone knows someone who has had the coronavirus or has been sick from it themselves. The major impact of the virus also drew a lot of attention from researchers. Vaccines were developed in record time, but other fields of research also developed enormously. An example of this is the development of mini-lungs for research into the coronavirus. But how do these so-called organoids actually help us in research into viruses? Why are they such a valuable addition? And could they perhaps one day be a replacement for laboratory animals?
Scientists have been researching viruses for years. They are invisible to the eye, yet always among us. For example, every year there is a flu wave and many people receive a standard call for the flu shot. Over the years, researchers have developed various ways to mimic a virus infection in the lab so that they can better understand what happens in the body when someone is sick. Mimicking an infection is done, for example, by infecting cells in the lab with viruses or, when it comes to drugs and vaccines, using laboratory animals to investigate their effectiveness. These ways of mimicking infections can provide a lot of information about viruses, but they also have their limitations. For example, most of the cells that researchers use in the lab are not exactly the same as the cells in our bodies. As a result, scientists can never be completely sure whether what they see in the lab also happens in the body in exactly the same way. Scientists can often already make a better comparison with humans with laboratory animals, but there are still differences that create uncertainty within the research.
To overcome this problem, scientists are frantically searching for new ways of research. One of the labs that is working hard to develop better ways to mimic the human body for research is Hans Clevers’ lab. About 15 years ago, he accidentally grew the first ‘mini-organs’ in his lab. Tiny intestines that are almost invisible to the naked eye. Despite their small size, they mimic the organs in our body extremely well and the cells they consist of are exactly the same as the cells in our body. Now, some 15 years later, the Clevers lab already has much more than just mini-intestines in culture that are used for a lot of different research. An example of this are the mini-lungs that Jelte van der Vaart, a researcher in the Clevers lab, developed last year together with his colleagues for use in research into the coronavirus.
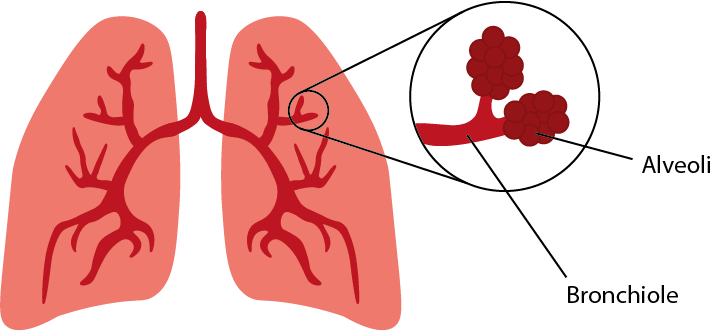
Drawing of the bronchioles and alveoli.

Difference between single cells and an organoid: A cell culture consists of one type of cell that spreads randomly over the bottom of a dish. An organoid can consist of several types of cells and the cells together can take a certain shape.
The mini-lungs that Jelte developed mimic two types of tissues in the lungs: the bronchioles and the alveoli. Bronchioles are tubes in the lungs that carry air to the alveoli. The alveoli look a bit like balloons that ensure that oxygen from the air can be absorbed into the blood. The alveoli and bronchioles each consist of different types of cells. With the organoid technique, scientists grow the cells in such a way that a good composition of different cells is created and they mimic the tube and balloon structure of the lung in 3D. This is a major improvement over the classical research method in which scientists only use one type of cell for their research. Although the organoids can only be 1 millimeter in size, they already resemble the lungs in our body.
Scientists suspect that a coronavirus infection in the alveoli and bronchioles can cause severe inflammation. Due to these inflammations, our body can absorb oxygen less well, which causes an oxygen shortage. “We have copied the first layer of cells that the virus encounters in the alveoli and bronchioles, so we can focus on the question: what happens at the moment of the first infection,” says Jelte. He and his colleagues have been able to show that the coronavirus can indeed easily infect these types of cells. They have also already taken the first steps in testing drugs on the mini-lungs. They tested a drug suspected of inhibiting the spread of the virus, and indeed it did.
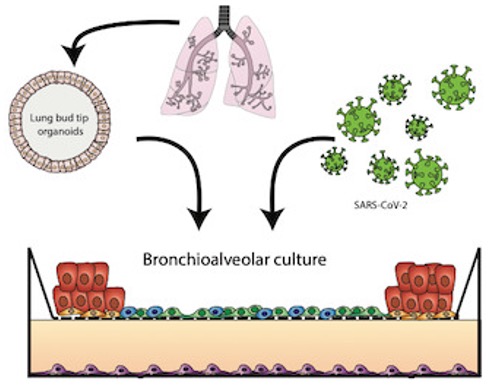
Picture from Jelte his article. He and his colleagues make small lung organoids by taking a few cells from a human lung and growing them further in the lab. The researchers then infect the lung organoids with the coronavirus, after which they can use a microscope to see what happens to the cells.
Testing medicines like Jelte has done is one of the fields in which organoids can be of great significance. At present, researchers still make extensive use of laboratory animals, but the organoid technique is a promising replacement. “I think that organoids can almost completely exchange laboratory animals. If you look at the research we are already doing with the mini-organs, we are already doing this for many animal experiments. I don’t expect that we can do without it completely, because we mainly look at the cells that are infected by the coronavirus. Cells of our immune system react to this again and we should also be able to view this reaction, for example, you probably need laboratory animals for this,’ says Jelte. Scientists can therefore very well test the first steps in research into new or existing medicines and their effect on a clinical picture with the mini-organs. Only with the next steps in research into their effectiveness, laboratory animals come into play again.
Mini-organs can therefore mean a lot in research into viruses and medicines, especially because they resemble the tissues in our own body. This ensures that we can make the translation to the human body easier. But Jelte does not only want to apply the technique in these fields, he also hopes, for example, that it can be used in organ transplantation in the future. All in all, these so-called mini-organs seem to have a multifaceted future and there’s a good chance we’ll be hearing a lot more about them!
References
https://www.embopress.org/doi/full/10.15252/embj.2020105912
https://www.hubrecht.eu/nl/model-ontwikkeld-voor-onderzoek-naar-sars-cov-2-infectie/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8272930/
Interview with Jelte van der Vaart (12-10-2021)
This page was translated with Google Translate.

