A Gut Feeling
Thinking about your gut means thinking about your brain
Thinking about your gut means thinking about your brain
(The brain and the gut: two organs far away from each other, but still able to communicate. iStock. ID 1316665852. 2021)
A recent link that researchers have made is that between mental health and the gut microbiota; the collection of microorganisms existing in our intestines. Researchers have shown that people suffering from depression and anxiety also had disruptions in their gut microbiota. But how exactly this works is not known, so researchers are investigating this link and if it can be used for treating these problems. This is important since mental health issues like depression and anxiety are globally on the rise since the start of the pandemic, especially in teenagers and adolescents.
Purpose of the gut microbiota
The gut microbiota mainly houses bacteria, but other ‘microorganisms’ like viruses also exist there. Bacteria and viruses in our bodies may not seem like a positive note, but these ones help our bodies with the digestion of food. Without them, the uptake of much needed nutrients would not work as good and efficiently as it does now. There are even estimations saying that there are more bacteria and viruses in our gut than the number of cells in our body.
But for the gut microbiota to work best the microorganisms need to be diverse and well maintained. This can be done by eating certain foods, for example by eating vegetables or food high in fiber. A poor diet can result in a so called ‘disruption’ of the microbiota, which can have a negative impact on your body.
Where it goes wrong
The negative impact of a disrupted gut microbiota was also what researchers investigating mental health were able to show. Tests in people suffering from mental health problems like anxiety do show less diversity when compared to people not suffering from these ailments. Researchers did further tests in animals to investigate if changes in the gut microbiota can directly affect your mood to see if it can be a cause for these mental problems. In one example, researchers from China showed that changes in the gut microbiota of mice caused anxiety and depression-like behavior and changes to the brain.
Researchers propose that the idea behind this interaction is that the gut and the brain are able to communicate with each other. They can do this by releasing certain proteins into the bloodstream which can reach the other organ and affect their functioning. This communication works both ways, meaning that both organs can affect the functioning of the other
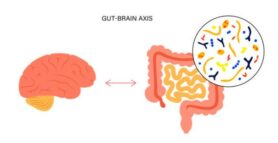
The Gut-Brain-Axis is the name for the connection between the brain and the gut. The microorganisms (represented as the drawing inside the circle) are capable of releasing proteins into the bloodstream, which can reach the brain and be used to relay information. This can for example be useful when your body is low on energy; the brain can then ‘tell’ the gut to take up more nutrients to increase energy. (iStock images. ID 1351744853. 2021)
Where it can go wrong is that a disrupted gut microbiota (due to an unbalanced diet) can have a negative impact on your mood via this way of communication. Researchers think that this can (partially) cause mental health issue like depression and anxiety. However, this way of communication is quite complex so more research is currently been done to fully understand it all.
Improving gut means improving mental health?
The question then becomes if taking care of a disrupted gut microbiota will also lead to improved mental health. Does a diverse microbiota automatically mean clearing these problems? Research does show that a diverse diet containing lots of fibers, vitamins and minerals (and somewhat low in fat) does improve the gut microbiota, but only improves mental health to a limited extent. Some researcher do show significant changes in overall mood and stress levels after following a specific diet, but not in everyone and some studies do not show significant changes. So no, improving your gut microbiota does not automatically mean clearing these problems.
Important to note is that this link between microbiota and mental health is seen as a possible cause for mental disorder, but not the only one. These disorders are quite complex in nature and their cause is linked to different things happening in your body and your life(style). Changing one thing does most of time not result in immediate effects for everyone, but can be a step in the good direction and show promising results for some.
What it means for you
More research is currently being done to investigate this link quite complex link between the brain and the gut, what it means for people suffering from mental health problems and what specific diets and lifestyle changes can mean for us. For now, watching your diet and maintaining a healthy lifestyle are good things to always keep in mind. This is especially true for people at a young age, since their body, and gut microbiota, are growing. This means that a disruption can more easily have a big and negative impact.
If you’re interested in learning more about what a good diet and lifestyle is for your gut microbiota then read our other articles regarding ‘the gut microbiota and nutrition’. If you want to know more about what other disorders a disrupted microbiota is linked to then read our articles on ‘gut microbiota and colorectal cancer’ or ‘gut microbiota and autism.
References:
Park, M., Choi, J. and Lee, H.-J. (2020) ‘Flavonoid-Rich Orange Juice Intake and Altered Gut Microbiome in Young Adults with Depressive Symptom: A Randomized Controlled Study’, Nutrients, 12(6). doi:10.3390/nu12061815.
Images from iStock
Second Image: https://www.istockphoto.com/nl/vector/gut-brain-connection-gm1351744853-427385084

