The development of artificial organs
A mini brain with eyes
Written by Tara Wingelaar
Growing artificial eyes with your own DNA in a lab. This sounds like an interesting futuristic scenario, but this is already being done in labs. A research team from the Heinrich Heine University in Düsseldorf has recently grown small brains in the laboratory that can also grow eyes. The eye structures work exactly as they do in the human brain: they respond to light by sending signals to the mini brain. Very cool, an artificial mini brain with mini eyes that is also functional, but what good is it? And could it possibly mean something for patients with eye diseases?
Doing research with the mini brain
The cultured mini brain with eyes forms a 3D structure (or: ‘organoid’) that is very similar to how your eyes connect to your brain. Just like with your eyes, the light enters the eye through the lens. After this, it falls on the back part of the eye: the retina. The retina then sends the incoming information, via the optic nerve, to the brain. They process the information and ensure that you can see.
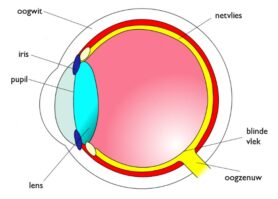
Schematic representation of the eye
Because the brain organoid with eyes is so similar to the real situation, it can be used for research, for example, into the development of eye diseases. Research into eye diseases is now mainly done using animal experiments or in 2D tissues. Both methods contributed greatly to this research, but the 3D mini brain seems to best mimic the human brain.
Treatment of eye diseases
Another important advantage of the brain organoid with eyes is that patients with eye diseases could receive tailor-made treatment. A personal mini brain can be made for each patient. The main ingredient needed to grow the brain organoid are stem cells. These cells are a kind of basic cells that contain the unique properties of the patient themselves. This means that it is possible to investigate for each patient how they will respond to certain medicines and which external factors influence the disease.

The mini brain with eyes in a 3D structure, a few millimeters in size
This could, for example, be performed with patients diagnosed with the eye disease glaucoma, which is diagnosed in about 2 in 100 people over the age of 45. In this disease, the eye pressure rises because drainage channels in the eye are clogged for example. You only notice the rising eye pressure when it is already too late: it oppresses the optic nerve and has an effect on your vision. ‘You cannot reverse the damage that has already been done,’ says Laurien van Heukelom about the optic nerve that is irreversibly damaged in glaucoma. She has been working as an optometrist in an eye hospital for four years, so she has a lot of experience with patients with eye diseases such as glaucoma. Her father and grandmother have also been diagnosed with familial glaucoma, which means that she is also at high risk for the disease. From the age of 40 she will be examined by an ophthalmologist. It is important to detect the disease in an early stage because of the irreversible damage to the retina and optic nerve that cause limited vision. ‘There’s no treatment to improve those visual field defects, you’re just going to prevent it from getting worse. And I have to say that this is the case with many eye diseases,’ she says.
Treatment for patients with hereditary predisposition to glaucoma now mainly consists of prevention and stopping the worsening of the disease. The mini brain with eyes can contribute a lot to research into the origin of this disease and provide tailor-made treatment.
“It is very limiting if you are or know that you will become visually impaired. Very scary and frustrating.”
Artificial eyes for transplantation
But of course you would prefer to tackle the cause of the vision loss in glaucoma: the damage to the retina and the optic nerve. To this end, the researchers of the mini brain propose that the artificial eyes could possibly be used for transplantation in the future. For example, of the retina and optic nerve of patients with glaucoma.
In the past, research has been done into transplanting a donor retina. But because this is foreign material, it is often rejected by the patient undergoing the retinal transplant. Making the connection between the new retina and the optic nerve is also an obstacle. The cultured mini brain to which the eyes are already attached would offer a solution here. There is therefore no longer the question of rejection because it has been cultured from the patient’s own stem cells. If the technique for growing artificial eyes were further developed and improved, it could possibly offer a solution for many people with limited vision due to eye diseases such as glaucoma.
Translated from Dutch
Sources
Ducheyne, P., Grainger, D. W., Healy, K. E., Hutmacher, D. W., & Kirkpatrick, C. J. (2017). Comprehensive Biomaterials II. Elsevier Healthcare.
Gabriel, E., Albanna, W., Pasquini, G., Ramani, A., Josipovic, N., Mariappan, A., Schinzel, F., Karch, C.M., Bao, G., Gottardo, M., Suren , AA, Hescheler, J., Nagel-Wolfrum, K., Persico, V., Rizzoli, SO, Altmüller, J., Riparbelli, MG, Callaini, G., Goureau, O., . . . Gopalakrishnan, J. (2021). Human brain organoids assemble functionally integrated bilateral optic vesicles. Cell Stem Cell, 28(10), 1740–1757.e8. https://doi.org/10.1016/j.stem.2021.07.010
Levin, L.A., & Albert, D.M. (2010). Ocular Disease. Elsevier Healthcare.
Macular degeneration. (2021). Oogfonds.nl. Retrieved on October 20, 2021, from https://oogfonds.nl/oogspreis/maculadegeneration/treatment-maculadegeneration