Puberty
The future of male contraception
By Kelly Rademakers, April 6 2022

Despite its negative side effects, the hormonal pill is still the most popular method of contraception among young people. American research teams found two new possible forms of hormone-free contraception in the past weeks. Unlike most methods, these focus on making the man, rather than the woman, reversibly infertile. The researchers have successfully stopped the production and swimming of sperm cells. The next step is to test these inventions in humans and rule out possible side effects. The ultimate goal: a form of contraception freely available to everyone, without hormones.
Scientists have succeeded in making human sperm infertile with an antibody. Researchers from Washington State University announced this on the university’s website on February 7th. Normally, the structure of sperm changes after ejaculation. The initially gel-like structure becomes thinner and more fluid, allowing the sperm cells to swim. The antibody specifically inhibits this structural change in the sperm. This prevents the sperm cells from moving to be able to fertilise an egg cell. On the website, the researchers say that the new drug can be used in combination with condoms to increase the reliability of condom use. The team is now investigating whether their antibody can become a widely used form of contraception without causing unwanted side effects.
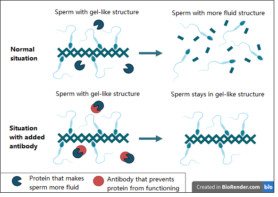
Figure 1. Sperm undergoes a structural change after ejaculation. It becomes more fluid, allowing the sperm cells to swim and search of an egg cell. The antibody studied by Washington State University ensures that this structural change does not occur. When it is added, the sperm remains in a gel-like structure. This prevents movement of the sperm cells and therefore fertilisation.
Additionally, the University of Minnesota has developed a hormone-free male contraceptive pill that has been shown to be 99% effective in mice. This is what Abdullah Al Noman, who collaborated on the invention, told the American Chemical Society on 23 March. With that, the reliability of the newly invented pill is equivalent to that of the female contraceptive pill. The high effectiveness was achieved after four weeks, during which the mice were given the male pill every day. For the production of sperm vitamin A is required, which is then converted into retinoic acid. Noman and his team’s pill prevented the conversion into retinoic acid, thus preventing the production of sperm cells. When the male mice stopped taking the pill, they had their full fertility back after 4 – 6 weeks. Moreover, no side effects were seen in the mice during the entire testing process. The application to test the men’s pill in humans is now underway, and the team hopes to start testing in late 2022.
Current contraceptive methods
Currently, condoms and sterilisation are the only reliable contraceptive options for men. Often, the pull-out method is not mentioned as an option due to its low reliability. In more than 1 in 10 cases, this method does lead to pregnancy. In the Netherlands, sterilisation is only rarely performed in men under 25. Doctors are often reluctant to perform this irreversible procedure on young patients. This is because the risk of regretting the sterilisation procedure later in life is greatest for men aged under 30. Research by Sexuality Expertise Centre Rutgers has shown that 70% of the Dutch adolescents use a condom the first time they have sex. However, 50% of adolescents who used a condom stopped using it within one month. In the case of a onenightstand, 40% do not use a condom. This means, in most cases, the responsibility for contraception lies with the women.
In most cases, young women still choose to use a hormonal contraceptive pill. In 2017, this amounted to 64% in the Netherlands, according to a report by Rutgers. It makes sense that the use of these methods among young people is so high. “This is because most children know very little about different forms of contraception,” says Hester van Dam, former sex education officer at secondary schools. “Often, they only know about the male condom and the pill.” Though, the lack of knowledge about contraception among young people is quite worrying. Hester: “Through the internet, adolescents have much more access to sex than was the case 15 years ago. As a result, they often know a lot about the physical aspect, but very little about safety and contraception. They are not aware for instance, that some methods of contraception contain hormones and others do not.”
Negative effects of the pill
The hormonal contraceptive pill causes negative physical and mental side effects for some users. This is due to the fact that you take in artificial versions of hormones through the pill, which reduce the natural production of hormones. For example, the hormones estradiol and progesterone, which naturally fluctuate during the month, are kept at a permanently low level when using the pill. These hormones affect areas of the brain that are important for the processing of your emotions. Additionally, testosterone levels are also lower than they would naturally be when taking the pill. A low level of testosterone is the reason some pill users experience feelings of depression and a low libido. So these hormones do not only have a function in the sexual organs, but also in the brain. Shutting down the natural fluctuation of these hormones and replacing that cycle with synthetic versions of hormones can therefore have far-reaching consequences.
General practitioner Marieke van Rijnsoever has noticed a decline in the number of pill users. The main reason for this shift is dissatisfaction with the hormones and their side effects, says van Rijnsoever. She makes sure to discuss the potential side effects when a patient considers taking the contraceptive pill. Marieke: “I particularly discuss the risk of thrombosis and the long-term risk of breast cancer”. She deems new hormone-free, reversible forms of contraception interesting and certainly desirable.
Van Rijnsoever also notes that parents often have an influence on their child’s choice of contraception. So it can be very helpful to talk about the pros and cons of various methods of contraception. Puberty is an important life period, full of hormonal changes. So new hormone-free contraception is a godsend to avoid negative side effects during this turbulent time. However, more research is needed before these new forms of contraception appear on the market. So until they are available in shops, it is important to talk about the contraceptive options that are already available, so your child can make an informed choice. That difficult choice will hopefully be expanded in the near future with these two newly researched forms of hormone-free contraception.
Sources
- Methoden van anticonceptie en hun betrouwbaarheid – Stichting Anticonceptie Nederland https://www.anticonceptie-online.nl/methoden.htm
- Actieplan ‘Seks onder je 25e’ – Rutgers expertisecentrum seksualiteit
- Gupta, S., & Kumar, A. (2017). The human semen. In Basics of Human Andrology (pp. 163-170). Springer, Singapore.
- Montoya, E. R., & Bos, P. A. (2017). How oral contraceptives impact social-emotional behavior and brain function. Trends in cognitive sciences, 21(2), 125-136.
- Website ‘Onderzoek naar de pil’ – onderzoeksteam van Estrella Montoya, Universiteit Utrecht https://onderzoeknaardepil.nl/onderzoek-naar-de-pil
- Weemhoff, M., Dewilde, D., & Hamerlynck, J. V. T. H. (2013). 19 Definitieve anticonceptie. In Gynaecologie (pp. 241-251). Bohn Stafleu van Loghum, Houten.
- Trapping sperm in semen’s natural gel could lead to new contraceptive – Washington State University https://news.wsu.edu/press-release/2022/02/07/trapping-sperm-in-semens-natural-gel-could-lead-to-new-contraceptive/
- A non-hormonal pill could soon expand men’s birth control options – American Chemical Society https://www.acs.org/content/acs/en/pressroom/newsreleases/2022/march/non-hormonal-pill-could-soon-expand-mens-birth-control-options.html
- Interview with researchers of University of Minnesota on their research by American Chemical Society https://www.youtube.com/watch?v=GsBQ9Obgv1Y&list=PL-qHxGvFeZV0XKumlYsVz0aI_l_EwgKU0&index=12
- Aantal ziekenhuisopnamen en –patiënten diagnose sterilisatie – CBS https://www.cbs.nl/nl-nl/cijfers/detail/84067NED?q=sterilisatie

